Making the difficult decision
When curvatures are over 40 degrees, most physicians will recommend corrective spine fusion surgery. This does NOT mean surgery is a necessity. Please consider getting several orthopedic opinions and most importantly from a spine specialist whose primary caseload is scoliosis.
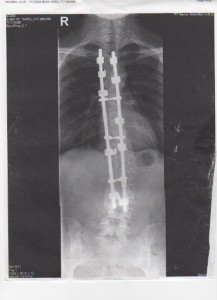
Photo of Julie Wilkins post surgery. Fused from T3-L3 with Cottrell Dubosset instrumentation. Notice the remaining lumbar curve which measures approximately 23 degrees.
The goals of scoliosis surgery are threefold:
- Mechanically straighten and derotate the spine as much as safely possible
- Balance the torso and pelvic areas
- Maintain the correction long-term
It takes a two-part process to accomplish these goals:
- Fusing (joining together) the vertebrae along the curve
- Supporting these fused bones with instrumentation (steel rods, hooks, and other devices) attached to the spine
This decision is never an easy one to make. Many times the patient is not in pain, is healthy, and active. Sometimes surgery is delayed during adolescence, and then the individual decides to go forward with corrective surgery in adulthood. It is well known that children fair better, recover faster, and tolerate surgery better than adults do. Age has a great impact on ease of recovery.
Here are some questions to ask your physician as you are making this decision:
1. What levels of the spine will be fused ? This is important to know. Google a good spinal anatomy picture or visit my video tutorial HERE and familiarize yourself with vertebral levels. Most scoliosis fusions start between T2-T4 and travel down as far as L3 or L4. This leaves the neck fully mobile and the very bottom of the spine with some mobility. The further down the fusion is, the less lumbar vertebrae remain to carry the weight bearing load. We are seeing heavy disc degeneration years post fusion in the lumbar vertebrae in those fused to L3 or L4. My opinion is the more lumbars that are left untouched the better the outcome, although this will be a discussion for you and your orthopedic surgeon.
2. What type of rods and screws will be used ? The hardware for spine fusion surgery has evolved over the years. The early use of the Harrington Rod, left many with flat back syndrome as well as other poor surgical outcomes requiring revision surgery. Currently there are many types of hardware as well as special screws that help facilitate correction of spinal rotation. Ask your surgeon what type of hardware is being used, how long he/she has been using that type of instrumentation, and if there will be rotational correction.
3. Where does the bone graft material come from to create the fusion ? Bone may be harvested from the body or donor grafts can be used. Bone from the patient's body (rib cage, hip, or spine) is the best quality bone. Keep in mind fusion STOPS growth of the fused bones. If children have not reached their maximum height, the spine will no longer grow. The remaining growth spurts will be in the extremities and not in the fused spine. Ask your doctor to assess if the child has finished growing, and have some discussion over waiting until the growth is complete vs fusing when height may still be attainted.
4. What kind of precautions/limitations will I experience after surgery and for how long ? Most of the time the patient is to be resting and taking it easy for the first 3 months after surgery. Most school aged children will schedule the surgery in early summer to be able to return in the fall. It usually takes 3-6 months for the vertebrae to fuse, and there will be movement restrictions during this time. Once fused, spinal curvature and rotation can no longer take place, however the spine may still curve above and below the fusion. Once fusion occurs, the rods are not really needed, however they remain in the body unless complications or infection occur. It is worth asking your physician how many revision surgeries he has performed to assess his surgical outcomes.
5. How do we prepare for surgery ? Before the operation, a doctor conducts a complete physical examination to determine leg lengths, muscle strength, lung function, and any postural abnormalities. The patient receives training in deep breathing and effective coughing to avoid lung congestion after the operation. The patient should also receive training in turning over in bed in a single movement (called log-rolling), before the operation. Psychological intervention, using cognitive-behavioral methods that help young patients cope, may be very helpful in reducing anxiety and pain after surgery.
Patients are encouraged to donate their own blood before the operation, for use in possible transfusions. The patient should be healthy going into surgery. Optimum nutrition and /or supplements should be considered in preparation for surgery.
6. How do I prepare for the transition home after surgery ? You can expect the patient to need full care in the weeks following surgery. They will need assistance getting in and out of bed, using the bathroom, and bathing. A shower seat and elevated toilet with arm rails would be helpful to have upon arriving home. Patients will usually be sitting up the day after surgery. Physical Therapists will likely be ordered to assist in sitting up and walking in hospital. The patient should be walking around independently within a couple of days to week. There is a lot of stiffness after surgery and this takes a while to subside. There will also be some unusual sensations in the back such as tingling, twitching, and burning as the nerves regenerate. This can be felt all through the first year.
Typically a couple of inches of height are gained and the patient may notice this immediately. It may take a year or more for muscle strength to return so patience is definitely needed during this recovery time! There can also be some post surgery anxiety and depression which is quite common.
You may notice some "settling" in the back that occurs in the months after surgery. Sometimes it might appear that the curve is returning. It is likely that the surgeon left some curvature in the spine as it is rare to get 100% correction. The "settling" is the muscles and tissue softening back into a place of comfort. Try not to worry about this as it is all part of the body readjusting to its new postural alignment.